
The key to effecting public policy change in healthcare is to be persistent, patient, and focused, says Michael R. Cohen, president of the Institute for Safe Medication Practices (ISMP).
“We try to make everything about patient safety,” Cohen said on September 25 while delivering the 2018 William A. Zellmer Lecture in Bethesda, Maryland, during ASHP’s annual Policy Week. “No one wants to see a patient get hurt.”
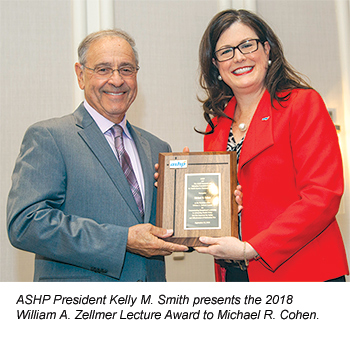 Cohen is the ninth recipient of the William A. Zellmer Lecture Award, which was established by ASHP and the ASHP Research and Education Foundation to recognize leadership in advancing public policy that promotes safe and appropriate medication use. The awardee delivers the lecture as part of ASHP’s annual Policy Week activities, during which ASHP members—nearly 100 this year—visit their elected officials on Capitol Hill to advocate in support of the vital roles pharmacists play as patient care providers (see sidebar on page 1842).
Cohen is the ninth recipient of the William A. Zellmer Lecture Award, which was established by ASHP and the ASHP Research and Education Foundation to recognize leadership in advancing public policy that promotes safe and appropriate medication use. The awardee delivers the lecture as part of ASHP’s annual Policy Week activities, during which ASHP members—nearly 100 this year—visit their elected officials on Capitol Hill to advocate in support of the vital roles pharmacists play as patient care providers (see sidebar on page 1842).
During his lecture presentation, Cohen told the more than 150 pharmacists and others in the audience that their efforts have been integral to ISMP’s successes over the years.
For example, he said, the United States Pharmacopeia general chapter on prescription container labeling “really started with reports that you sent to ISMP and to FDA to tell us about things that were problematic with the label,” such as abbreviations.
He said ISMP has also worked closely with FDA, the Centers for Medicare and Medicaid Services (CMS), the Centers for Disease Control and Prevention, the Joint Commission, and other healthcare and regulatory stakeholders, including ASHP, to drive important policy changes.
But he emphasized that ISMP has no regulatory or enforcement authority—it is a nonprofit entity, staffed by clinicians, with a sole focus on patient safety.
He also said that policy change is best accomplished through gaining the commitment of frontline staff to follow demonstrably safe practices and not by simply demanding compliance.
“So many times, the recommendations may be out there but the people that actually have to implement them don’t necessarily understand why these recommendations are in place,” he said.
Cohen said the actions of a single person can lead to big medication safety improvements. He recalled the work of pharmacy automation consultant Mark Neuenschwander, who encountered Cohen at an ASHP meeting and talked about how barcode technology could prevent medication administration errors.
That conversation, he said, helped spur regulatory action from FDA and promote policies “to put bar coding on every item that touches the drug,” including unit dose syringes.
Cohen noted that it took far more than 1 person to drive change to the so-called 30-minute rule, a CMS policy that ISMP had declared unsafe for patients. An ISMP survey of 18,000 nurses indicated that the rule, which required that all inpatient medications be given within 30 minutes of the scheduled administration time, drove nurses to use potentially dangerous workarounds to avoid being cited for noncompliance.
The CMS rule applied to all medications, including those for which the timing of administration isn’t clinically relevant.
“It just didn’t make sense,” Cohen said.
CMS abandoned the 30-minute rule in 2011 in favor of recommendations promoted by ISMP. A CMS guidance document cited the ISMP survey and acknowledged that the 30-minute rule was “no longer the standard of practice in the current hospital environment.”
“We were very fortunate to see that happen,” Cohen said of the decision.
ISMP has also been working with FDA for years to promote packaging configurations that discourage diversion of opioid-containing products. Cohen said the effort was driven by multiple reports from pharmacy customers that they were being “shorted” when having prescriptions for opioid drugs filled.
“They would go to a pharmacy, and they were supposed to get 40 units of Vicodin tablets on their prescription. And when they got home they counted them, and there were just 29,” suggesting possible diversion by pharmacy staff, he said.
To combat the problem, ISMP recommended using blister packaging for opioid-containing products and limiting prescribing to a few days’ supply for patients with acute pain. Cohen said such packaging is standard in certain other countries.
Days after Cohen spoke, Congress passed bipartisan legislation—the SUPPORT for Patients and Communities Act—that includes those provisions.
 Cohen said ISMP is currently involved in a project to ensure that pharmacy information systems display both the branded and generic names of medications. He said that many of the pharmacy information systems designed for ambulatory care settings display “only the brand name or the generic name but not both.”
Cohen said ISMP is currently involved in a project to ensure that pharmacy information systems display both the branded and generic names of medications. He said that many of the pharmacy information systems designed for ambulatory care settings display “only the brand name or the generic name but not both.”
ISMP has received reports describing incorrect outpatient medications that were dispensed because of the naming limitation. Cohen said technology vendors have been responsive to this problem and are starting to make changes that address ISMP’s concerns.
Cohen predicted that changes will occur in other important patient safety areas, such as requiring healthcare organizations to proactively assess whether they are at risk for errors that have been reported at similar institutions.
He also said it’s likely that compounding facilities will replace “human-readable labels” with technologies that track the manipulation of sterile products throughout the entire compounding process.
And he suggested that there will be increased scrutiny, driven by reports from consumers, of medication safety in community pharmacies.
“We have not seen a lot of pickup of patient safety medication safety topics in community practice, especially in the larger chains. We see the same errors [repeated] time and again,” he said.
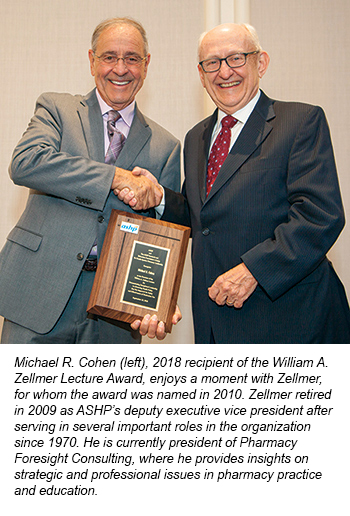
Zellmer Lecture Sets Tone for Policy WeekSince its inception in 2010, the annual William A. Zellmer Lecture has energized pharmacists from across the country during ASHP’s Policy Week, held this year September 24–28. The lecture is delivered the day before the pharmacists visit their legislators on Capitol Hill to advocate for policies that advance the pharmacy profession and improve patient care. Policy Week participants include members of ASHP’s 5 policy councils and the Commission on Affiliate Relations, who convene to discuss pressing issues and make recommendations that guide ASHP’s advocacy and outreach efforts. Key issues and discussion topics this year included pharmacists’ role in suicide prevention, artificial intelligence and machine learning, management of emergency supplies of medications during catastrophic events, naloxone as a discharge medication, therapeutic use of cannabidiol oil, and support of the pharmacy technician workforce. |
[This news story appears in the December 1, 2018, issue of AJHP.]








