Amid America's ongoing battle against opioid addiction, two pharmacists have worked at the forefront of a compassionate approach that aims to change how patients are treated.

Terri Jorgenson provides consultation and resources for a vast network of more than 6,000 Veterans Health Administration clinical pharmacist practitioners (CPPs) who treat patients grappling with a range of health issues, including opioid use disorder. Meanwhile, Jeffrey Bratberg combines his efforts in research, policy, and teaching to enhance care for individuals using opioids.
Jorgenson and Bratberg, both ASHP members, want to change how people see and treat opioid use disorder. Their experiences reveal how complex the problem is and what drives them to make a difference in patient care.
A mission born from crisis
Jorgenson, national program manager of clinical practice integration and model advancement for the Veterans Health Administration Pharmacy Benefits Management Clinical Pharmacy Practice Office, was inspired to get involved in care for patients using opioids back in 2012. She was then working for a VA network in Texas and seeing data about increasing opioid-related overdoses.
“Opioids were hijacking families, the community, and the lives of our patients,” said Jorgenson. “It felt like one of the most dangerous times in healthcare and one of the biggest opportunities to make a difference…I felt very strongly that we had to do everything we could as a healthcare community to come together and really change that direction of pain care through new pain and opioid stewardship efforts and making sure our patients had access to the help they needed.”
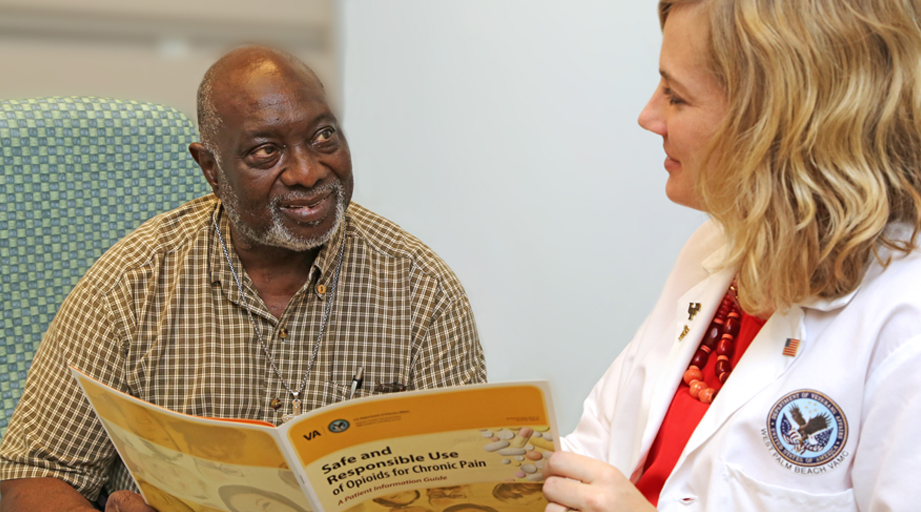
Today, she helps oversee and define scope of practice for the CPPs. These pharmacists provide comprehensive medication management to over 1.5 million veterans through a collaborative practice agreement, including prescribing and adjusting medications and ordering lab tests. They also provide overdose education and can offer naloxone, screen for suicide risk, and provide sterile syringes or drug test strips if appropriate.
Last year, CPPs prescribed and monitored medications for opioid use disorder for some 1,100 veterans.
“I love hearing the patient success stories, that they feel the work of their CPP and healthcare team is saving their lives, and sometimes their marriage or custody with their children,” Jorgenson said. “I really hope that what we’re doing in the VA encourages and empowers other healthcare communities and organizations to improve patient care and access to treatment through team-based care that includes pharmacist practitioners as key members of that team.”

Advocacy and education
Bratberg, who has critical care and infectious disease training, conducts research and teaches about opioid use disorder prevention, treatments, harm reduction, and increasing access to care across the cascade of care.
“No matter what setting you’re in, you’re going to experience people who use opioids,” said Bratberg, a clinical professor of pharmacy practice and research at the University of Rhode Island. “You’re going to need to promote the most proper use of these opioids and discuss lifesaving medications like buprenorphine and methadone…and connect people to medication services we offer and refer them to care for other drivers of health.”
Bratberg also educates others about the pharmacist’s role in providing care to people who use drugs and how to reduce the harms of illicit, unregulated opioid use. He’s helped write guidelines, assisted with revamping an opioid use disorder course, and presented his work at the ASHP Midyear Clinical Meeting & Exhibition.
“My career in public health is all about how we treat populations,” said Bratberg. “It’s also about treating each person in front of you like a human and not letting what society has told us about how we should treat people who use drugs affect our principles of human rights. That’s what I tell policymakers and pharmacy students and residents.”
Some of his work includes advocacy and helping write responses to government policy. “That’s really where the change is,” he said, “because if we can change policies, then we potentially change how society treats people, and then people have a better chance to get better.” The widest gaps in care can be closed by treating underserved, forgotten populations, said Bratberg, who hosts a public health-focused podcast called The Regimen. “We need less paternalistic medicine and much more patient-centered medicine. That really comes from the primary goal of harm reduction, meeting people where they’re at.”








