Digital enhancements to drug therapy offer a way to help patients stay on track with their treatment regimen and can potentially motivate them to lead healthier lives.
“Our patients have been very excited to use this technology,” said Rachel Drury, ambulatory care pharmacy coordinator for Froedtert Health in Milwaukee, Wisconsin. “This is a tool that we use, really, to help engage patients in their health.”
Froedtert Health last December began offering sensor-equipped formulations of cardiometabolic drugs to ambulatory care clinic patients who are at risk for cardiovascular complications. The technology records and transmits the time that each medication dose is taken and can also share data about the patient’s activity and self-reported health status indicators.
Placebo tablets containing the ingestible sensors—made by Proteus Digital Health, Inc., of Redwood City, California—are placed, along with the patient’s medication, into capsules by a Froedtert Health pharmacist.
Drury said the filled capsules may be larger than patients are accustomed to but are not unduly large. She said in early July that more than a dozen sensor-equipped medications were available to prescribers through the clinic’s formulary.
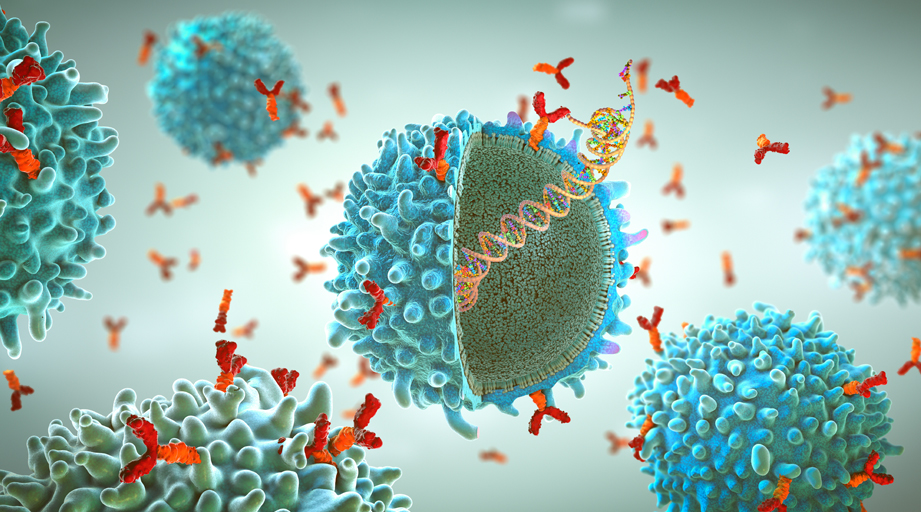
FDA classifies the sensor as an ingestible event marker. According to Proteus Digital Health, the ingestible sensor is activated during exposure to stomach acid and transmits a signal to a second sensor in a patch worn on the patient’s skin.
Data from the ingestible sensor are accessible, through a smartphone application and web-based portals, to patients and anyone authorized by them, such as a healthcare provider.
FDA’s approval of the application is limited to the portion that tracks ingestion of the drug.
The agency last fall approved the first-ever drug product that comes pre-equipped with a Proteus sensor. Abilify Mycite (aripiprazole tablets with sensor) is the result of a collaboration between Proteus Digital Health and Otsuka Pharmaceutical Co., Ltd.
According to Clinicaltrials.gov, the Proteus Digital Health sensors are also being evaluated in studies involving medications for the treatment of hepatitis C and HIV infection and as a potential alternative to directly observed therapy in patients with tuberculosis.
Drury said the sensor technology helps patients remember to take their medications. If a scheduled dose is missed, the application communicates that information to the patient and others who are authorized by the patient to receive the data.
And she said the adherence data, coupled with supplementary information that the application can track, help clinical pharmacists take better care of their patients.
“It really helps us get the data to be able to . . . make care decisions,” Drury said. “Clinical pharmacists . . . use the data to make many medication adjustments for patients.”
Such changes have included reductions in the dosages of antidiabetes medications for patients who adopt healthier lifestyle habits after using the sensor and the application to track their health status. The sensor technology has also allowed Froedtert Health’s clinical pharmacists to fine-tune metoprolol dosages to help patients improve their blood pressure control.
Drury said the sensor technology is provided to clinic patients at no additional cost and that Froedtert Health also uses the technology with medications for the treatment of hepatitis C.
“Froedtert Health is committed to finding ways to bring new technology to our patients,” she said. “Our big goal surrounding the technology is to help engage patients in their own healthcare.”
FDA in June announced the approval of another product that uses sensor technology—the Eversense continuous glucose monitoring (CGM) system by Senseonics, Inc., of Germantown, Maryland. The agency described Eversense as the first FDA-approved GCM system that includes a fully implantable sensor.
The subcutaneously implanted sensor lasts for up to 90 days. The sensor is wirelessly powered by a removable transmitter worn over the sensor site that sends glucose measurement data to a mobile device application.
The sensor reads blood glucose levels every 5 minutes. Patients must calibrate the system by performing a fingerstick blood glucose test twice daily.
Another new digital therapeutic product is reSET, a 12-week program that delivers cognitive behavioral therapy to patients undergoing outpatient treatment for a substance abuse disorder other than opioid dependence. The reSET program was developed by Pear Therapeutics of Boston and San Francisco and received marketing clearance in September 2017. The company states that the technology is the first prescription digital therapeutic with an FDA-cleared claim for the improvement of clinical outcomes in disease.
Baltimore-based WellDoc has also received FDA clearance for its digital product, the BlueStar mobile application. WellDoc describes the product as a digital therapeutic coaching tool for patients with type 2 diabetes.
Not yet approved is a video game–based digital product for improving attention, working memory, and inhibition in children with attention deficit/hyperactivity disorder. The software product is made by Akili Interactive Labs, Inc., of Boston. The company stated in April that it plans to file for FDA clearance of the technology in the coming months.
FDA has announced several actions intended to support the development of digital health technology products under the umbrella of the agency’s Digital Health Innovation Action Plan.
Last year, the agency launched a pilot program for software companies to precertify their organizations and potentially reduce or eliminate the need to file for regulatory approval of each specific device that uses their respective software products.
Last December, FDA released a guidance document that clarifies the characteristics of health-related software products that the agency doesn’t plan to regulate.
For example, software that identifies drug–drug interactions or drug–allergy contraindications on the basis of FDA-approved labeling would not be considered a medical device for regulatory purposes, according to the agency. And smartphone applications that encourage patients to adopt healthier lifestyle habits are also generally outside the scope of FDA regulation, according to another guidance document issued in December.
A guidance document that was released in April described how the agency intends to handle the approval of technology products that have a mix of components, not all of which fall under FDA’s regulatory authority.
[This news story appears in the September 1, 2018, issue of AJHP.]